In Parts one and two of this series, we focused on hormones used in contraception and why they are designed the way they are. Contraceptive hormones are engineered for one primary purpose: to suppress ovulation reliably and predictably. Menopause hormone therapy (MHT) is different - in formulations, dose, and intent. Understanding this distinction is key to moving beyond “hormones are good” or “hormones are bad,” and toward more personalized, evidence-based care.
Menopause Hormone Therapy Explained
In perimenopause and menopause, the goal of hormone therapy is not to suppress the hypothalamic–pituitary–ovarian axis, but to provide exogenous hormonal support that mitigates the effects of declining and fluctuating ovarian hormone signaling. Rather than suppression, the focus is on symptom relief and risk reduction - easing vasomotor symptoms, supporting bone and urogenital health, and improving quality of life in appropriately selected women. In short, the intent of menopausal hormone therapy is supportive rather than suppressive.
Because the goal is different, the formulation strategy is different. MHT focuses on estrogens (with or without progestogens) that more closely resemble endogenous hormones, delivered in ways that aim to achieve physiologic levels with minimal unnecessary metabolic impact.
Estrogens in menopause hormone therapy: how formulations evolved
MHT has gone through several distinct phases, each shaped by the same fundamental challenge: how to replace declining estrogen in a way that is effective, practical, and tolerable over the long term.
In the early decades of hormone therapy, clinicians worked with what biology offered. Naturally occurring estrogens such as estrone (E1), produced primarily by adipose tissue, estriol (E3), produced by the placenta during pregnancy, and estradiol (E2), produced predominantly by the ovarian follicles. They were identified and used clinically as early as the 1930s and 1940s. These hormones differed in their source and potency (estradiol being the most biologically active), but they shared a practical limitation: poor oral bioavailability. When taken by mouth, much of the hormone was rapidly metabolised, which is why early estrogen therapy often relied on injections rather than tablets.
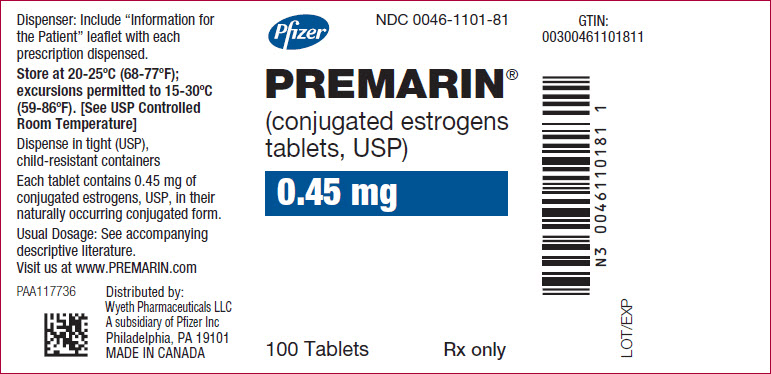
A major shift came in the 1940s with the introduction of conjugated equine estrogens (CEE). Researchers discovered that pregnant mares excreted high concentrations of estrogen in their urine, and these estrogens could be isolated, standardized, and taken orally with reliable effects. CEE offered something that earlier preparations struggled with: consistent absorption, predictable symptom relief, and scalable manufacturing. For decades, CEE became the dominant estrogen used in menopause therapy, and it remains in use today in products such as Premarin®.
Alongside CEE, other estrogen formulations continued to develop. Estradiol itself never disappeared, but it was often used in modified forms (such as estradiol valerate or estradiol acetate) to improve stability and absorption. Both estradiol acetate and estradiol valerate are estradiol esters. That means they are chemically modified versions of estradiol designed to improve stability, shelf life, and absorption. Once in the body, the ester group is cleaved, and the hormone becomes active estradiol. Estradiol valerate, in particular, was widely used in injectable hormone therapy, while estradiol acetate appeared in oral and vaginal preparations.
The modern era of MHT was shaped by a pivotal moment: the re-analysis of the Women’s Health Initiative (WHI) study. There was a renewed interest in using estrogens that more closely resemble endogenous human estradiol, particularly for systemic therapy, and in exploring delivery routes that minimise unnecessary metabolic effects.
Today, micronized 17β-estradiol has largely replaced estradiol esters for systemic MHT. Advances in pharmaceutical technology mean we can now deliver estradiol itself, via pills, transdermal patches, gels, and sprays, with reliable absorption and more physiologic hormone levels, without needing to modify the molecule.
Next-generation estrogens in MHT: where does estetrol (E4) fit?
Just as with contraception, the evolution of estrogens in menopause therapy reflects improving formulation science. One of the most closely watched developments is estetrol (E4). Estetrol is a naturally occurring estrogen produced by the human fetal liver during pregnancy. What makes it interesting for menopause therapy is not that it is “natural,” but that it has distinct estrogen signalling properties. Compared with estradiol, E4 binds more weakly to estrogen receptors and appears to activate a narrower set of estrogen pathways, with relatively less stimulation of hepatic, coagulation, and breast-related signalling. This selective activity is why E4 is sometimes described as a more “targeted” estrogen. Early clinical trials have shown that oral E4 can reduce moderate-to-severe hot flushes at defined doses, supporting its viability as an estrogen for systemic therapy. Larger ongoing studies are evaluating its effects beyond vasomotor symptoms, including quality of life, genitourinary symptoms, bone turnover, and markers of hemostasis. If approved for menopause indications, E4 would represent a new category of oral estrogen, distinct from both conjugated equine estrogens and estradiol. Importantly, it is not intended to replace transdermal estradiol, but rather to offer an alternative for women who prefer oral therapy and for whom estrogen selectivity may be advantageous.
Progestogens in menopause hormone therapy: protection, not suppression
In MHT, progestogens play a very different role than they do in contraception.
The goal of prescribing progestogens in MHT is not to suppress ovulation, but to protect the endometrium when systemic estrogen is prescribed to women with an intact uterus. This distinction is crucial because it explains both the choice of molecules and the doses used in MHT.
In the earliest days of hormone therapy, estrogen was often prescribed alone. It was only later, through clinical observation and epidemiologic studies, that it became clear that unopposed estrogen stimulated the uterine lining, increasing the risk of endometrial hyperplasia and cancer. This led to the introduction of progestogens in the 1970s, primarily to counterbalance estrogen’s effects on the endometrium.
Early solutions: synthetic progestins
The first widely adopted solution was the use of synthetic progestins, most notably medroxyprogesterone acetate (MPA). These compounds were orally stable, potent, and effective at providing endometrial protection. As with contraception, their appeal was largely practical: they worked reliably, were easy to manufacture, and fit well into oral dosing regimens.
Over time, a variety of synthetic progestins were incorporated into menopause therapy, including norethindrone acetate, levonorgestrel, drospirenone, dydrogesterone, and norgestimate, delivered via oral tablets, transdermal patches, an IUD, or combined formulations. Each offered slightly different receptor profiles and tolerability characteristics, but all shared the same primary function: preventing estrogen-driven endometrial proliferation.
A shift toward micronized progesterone
In the 1990s, oral micronized progesterone became available as a bioidentical alternative to synthetic progestins. Unlike synthetic progestins, micronized progesterone is molecularly identical to endogenous human progesterone. Advances in micronization technology made it possible to deliver progesterone orally with sufficient bioavailability to provide endometrial protection, something that had not previously been feasible.
This development marked a meaningful shift in menopause care. For the first time, clinicians could choose between synthetic progestins designed for potency and stability, and a bioidentical hormone designed to more closely mirror physiologic progesterone signalling.
Regimens evolved alongside formulations
It’s worth noting that the Women’s Health Initiative influenced not just which hormones were prescribed, but how they were prescribed. In response to WHI findings, clinical practice shifted away from cyclic regimens that induced monthly withdrawal bleeding and toward continuous combined therapy for many women. This change reflected a desire for simpler regimens and improved tolerability.
Comparative evidence across progestogens in MHT remains limited. Few high-quality trials directly compare multiple estrogen–progestogen combinations head-to-head, and available meta-analyses are constrained by heterogeneity in dosing, formulations, and outcome definitions.6-11 What can be said with confidence is that the choice of progestogen influences tolerability, bleeding patterns, and patient experience, even when the primary goal, endometrial protection, is achieved.11 More real-world data and research are needed in this field.
Putting it in context
From a physiological standpoint, although natural, menopause is a state of both estrogen and progesterone decline/deficiency. Progesterone production often declines earlier and more abruptly than estrogen as ovulation becomes irregular and eventually ceases. While the most clearly established, guideline-based role of progesterone in MHT remains endometrial protection, there is growing interest in its broader neurophysiologic effects, particularly its influence on sleep quality, mood regulation, and central nervous system signalling. These potential benefits are biologically plausible and supported by emerging observational and clinical data, but they remain an evolving area of research and practice.
Crucially, progestogens used in MHT are not interchangeable with those used in contraception, even when the same molecules appear in both settings. The dose, route of delivery, and therapeutic intent are fundamentally different. Contraception prioritises ovulation suppression; MHT focuses on restoration, prevention, symptom relief, and long-term tolerability.
(An important distinction is the levonorgestrel IUD, which can be used as a contraceptive as well as a progestogen in MHT, providing endometrial protection).
Micronized progesterone is now the preferred progestogen in many contemporary MHT protocols, reflecting a shift toward formulations that resemble endogenous hormones.
A brief note on “bioidentical” hormones
The term “bioidentical” is widely used and often misunderstood.
In clinical terms, bioidentical hormones are molecules that are structurally identical to the hormones produced by the human body. Importantly, all FDA-approved formulations of 17β-estradiol and micronized progesterone are bioidentical.
There is emerging evidence suggesting that bioidentical estradiol and micronized progesterone may offer advantages in certain outcomes, particularly thrombotic, metabolic, and breast-related effects, when compared with some older synthetic formulations. So far, this data comes from observational studies and mechanistic research as we await randomized trials (1-2).
Bioidentical MHT is not inherently “risk-free,” but it is increasingly favoured in modern MHT regimens because it more closely replicates endogenous hormone signalling and allows for greater individualisation.
Dose comparison: contraception vs menopause hormone therapy
Before we look at the numbers side by side, it’s worth addressing a common point of confusion. Hormonal contraception is typically dosed in micrograms (µg), while MHT is dosed in milligrams (mg). One milligram equals 1,000 micrograms. At first glance, that sounds like a huge difference. While the numbers look bigger with MHT, bigger numbers do not mean stronger hormones - they mean different design and different goals.
Potency vs physiology
Ethinyl estradiol, the estrogen used in most combined contraceptives, is a highly potent synthetic molecule. It binds strongly to estrogen receptors and is deliberately engineered to resist liver metabolism. This allows it to suppress ovulation at very low doses (15–35 µg).
By contrast, 17β-estradiol used in MHT is identical to the estrogen the ovaries produce. It is metabolized more quickly and does not exert the same amplified hepatic signal. As a result, higher oral doses (0.5 -- 2 mg) are needed to achieve physiologic replacement levels; or much lower doses when delivered transdermally (25–100 µg), which bypass first-pass liver metabolism altogether.
The same principle applies to the “huge” difference between micrograms of progestins and hundreds of milligrams of progesterone. Synthetic progestins used in contraception are designed for potency and durability. They bind strongly to the progesterone receptor, have long half-lives, and reliably suppress ovulation at microgram doses.
Micronized progesterone used in MHT, on the other hand, mirrors natural progesterone physiology. It has a shorter half-life, weaker receptor binding, and broader tissue metabolism. To provide endometrial protection and, in some cases, support sleep or mood, it must be given in much higher milligram doses.
Summary table comparing dosages and delivery of hormones in contraception and MHT.
Aspect | Hormonal Contraception | Menopause Hormone Therapy (MHT) |
Estrogen Dose | 15-35 μg Ethinyl Estradiol (oral pills, patch, ring) | 0.5-2 mg oral of microionized17β-estradiol or 25-100 μg transdermal estradiol |
Progestin/Progesterone Dose | 1-4th generation synthetic progestins, typically ~1000-3000 μg | Micronized progesterone, typically 100–200 mg daily |
Delivery | Oral, transdermal patch, ring, injectables | Oral, transdermal, vaginal |
Primary Goal | Ovulation suppression, menstrual cycle management, menstrual symptoms management, birth control | Restore physiologic hormone levels, relieve hypoestrogenic symptoms, support long-term health |
Quick counselling points
Different goals, different dosing: Hormonal contraception and MHT use hormones for entirely different reasons. Contraception is designed to suppress ovulation, while MHT aims to restore and maintain physiologic hormone levels as the ovaries wind down. The formulations and doses reflect those goals.
Progestins vs progesterone: In hormonal contraception, the progestin is the main driver of ovulation suppression, cervical mucus thickening, and endometrial changes that prevent pregnancy. Estrogen supports cycle control but cannot prevent ovulation on its own. In menopause therapy, progestogen is primarily used to protect the uterine lining when estrogen is prescribed, with some formulations that might also support sleep and mood. “In birth control, the progestin is doing the heavy lifting to stop ovulation. In hormone therapy, progesterone’s main job is to protect the uterus.”
Why estrogen type matters: The estrogen used in most birth control pills (ethinyl estradiol) is a highly potent synthetic hormone designed to work reliably at very low doses. The estrogen in birth control is engineered to survive the liver and be very potent. In menopause therapy, we usually use estradiol, which is identical to the estrogen your body naturally makes and is dosed to replace what’s missing, not override your system. “The estrogen in birth control is engineered to survive the liver and be very potent. The estrogen in hormone therapy is identical to your own and designed to behave more physiologically.
Conclusion
We’ve gone from “hormones are bad” to “hormones are the answer” remarkably fast. As with most things in medicine, the truth is more nuanced. The effects of exogenous hormone therapies depend on the molecule, the dose, the delivery, the timing, and the person taking them. Both contraception and MHT formulations have evolved alongside advances in endocrinology, pharmacology, and clinical evidence. Early formulations prioritized reliability and broad effectiveness; newer ones reflect a deeper understanding of hormone signalling, metabolism, and individual variability.
Modern research and hormone care should be asking the question: what is the right formulation for this person, at this stage, for this goal?
If this was helpful, we can go deeper in future articles - exploring how different hormone formulations may carry different risk profiles, what the emerging evidence suggests about bioidentical versus synthetic hormones. Comment and let us know!
Authors: Dr Paulina Cecula, Namrata Ashok. Reviewed and edited by: Dr Aaron Lazorwitz, Elena Rueda
References:
1. Foschi M, Groccia G, Rusce ML, Medaglia C, Aio C, Sponzilli A, et al. Estradiol and Micronized Progesterone: A Narrative Review About Their Use as Hormone Replacement Therapy. Journal of Clinical Medicine [Internet]. 2025 Oct 16 [cited 2025 Nov 28];14(20):7328–8. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC12565450/
2. Stevenson JC, Cust MP, Gangar KF, Hillard TC, Lees B, Whitehead MI. Effects of transdermal versus oral hormone replacement therapy on bone density in spine and proximal femur in postmenopausal women. Maturitas. 1991 Mar;13(1):95.


